How Does the Placebo Effect Work?
- Siddhi Patel
- May 11, 2024
- 6 min read
Imagine a world where simply believing in the effectiveness of a pill could cure your worst headaches, or where a doctor's confident reassurance could significantly ease your chronic pain. As unrealistic as this may sound, this is a real phenomenon that occurs unknowingly in patientswithin certain contexts.
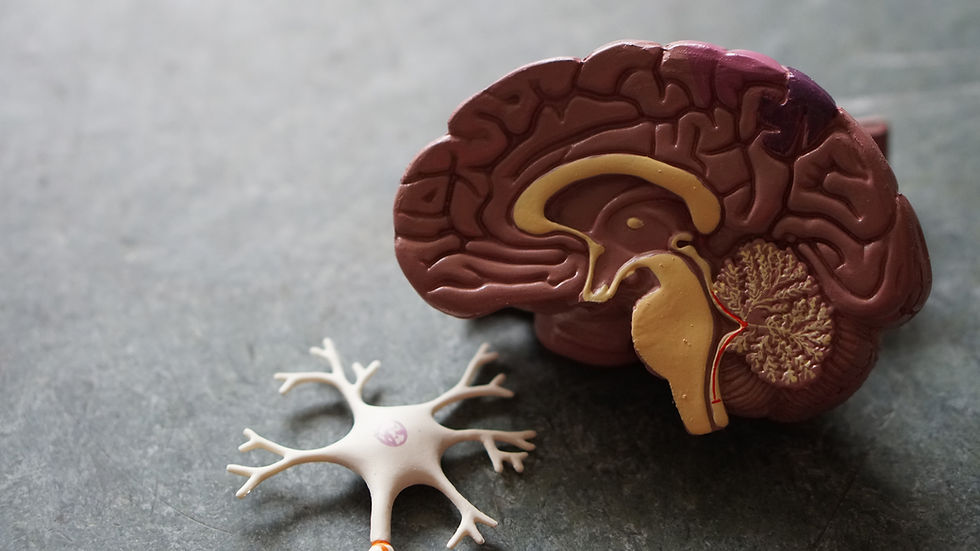
Known as the placebo effect, this fascinating occurrence shows the incredible power of our minds to influence our bodies. The placebo effect isn't just about sugar pills and deception; it's a gateway to understanding the complex interactions between our psychology and our physiology. But how exactly can an inert pill or treatment lead to real medical benefits, simply because we believe it will work?
What is the Placebo Effect?
The placebo effect is both a psychological and physiological phenomenon, where a patient's symptoms are alleviated by an inert or inactive treatment, simply because the individual believes that the treatment will help. Placebos themselves contain no active ingredient or active drugs meant to affect health; instead, they are usually made of substances like sugar pills, saline injections or even sham surgeries. Again, while these therapies mimic the visual of an actual treatment like a pill or surgery, they have no therapeutic effect on the individual.
Yet, in countless clinical trials, patients receiving these placebos report improvements in their condition, from reduced pain to alleviation of psychological symptoms like anxiety and depression.
The importance of the placebo effect goes beyond just helping individual patients; it's a vital part of medical research. Placebos are used to test how effective new medical treatments are. Researchers compare what happens to people taking a new drug against those taking a placebo to see if the drug’s benefits are real or just because people think they are taking real medicine.
Historical Context
The concept of the placebo effect isn't new. In fact, it has been around in medical practice for centuries. Historically, doctors often used treatments that were more about comforting patients than medically benefiting them, reflecting an intuitive understanding of the psychological aspects of healing. The term "placebo," Latin for "I shall please," was coined in the 18th century, referring to medicines given more to please than to benefit the patient.
The scientific exploration of the placebo effect began more earnestly in the 20th century. During World War II, the effect came into clearer focus when injured soldiers given saline injections—believed to be morphine—reported pain relief. This observation by Dr. Henry K. Beecher led him to further study and eventually publish a paper in 1955, titled "The Powerful Placebo." His work highlighted that across various studies, roughly 35% of patients showed improvement after receiving a placebo treatment. Beecher's findings propelled further research into how and why such effects occurred, prompting scientists and doctors to consider the psychological as well as physiological responses to medical treatments.
Mechanisms Behind the Placebo Effect
So how exactly does the placebo effect work? Researchers have identified several mechanisms, including neurobiological pathways, expectancy, conditioning, and suggestibility:
Neurobiology
One of the primary mechanisms by which placebos work is the release of endorphins. Endorphins are the body’s natural painkillers, chemically similar to opioid drugs. They bind to opioid receptors in the brain, which reduces pain and boosts feelings of pleasure. Studies involving placebo-induced pain relief have shown that the expectation of relief can trigger endorphin release, mirroring the effects of powerful pain-relieving drugs. This effect has been visualized in brain imaging studies, where placebo treatments lead to increased activity in brain areas known for their role in pain control, such as the anterior cingulate cortex, prefrontal cortex, and insular cortex.
Another neurotransmitter significantly involved in the placebo effect is dopamine. Known for its role in the brain's reward system, dopamine also contributes to how placebos can improve symptoms of conditions like Parkinson's disease and depression. The anticipation of a positive outcome (such as symptom relief) when receiving a treatment can increase dopamine levels, which not only enhances mood but also contributes to motor function and pain modulation.
Expectancy
The expectation of relief plays a critical role in how effective a placebo can be. When a person anticipates that a treatment will work, their brain sets into motion a series of reactions that can mimic real, pharmacological effects – similar to those explained in the neurobiological pathway. This expectation can be shaped by past experiences, the suggestions of a healthcare provider, or the perceived sophistication and cost of the treatment administered. The stronger the expectation, the stronger the placebo effect can be, illustrating how deeply our psychology can influence our physiological state.
Conditioning:
Beyond conscious expectation, conditioning is another powerful driver of the placebo effect. This occurs when the body subconsciously learns to respond to certain stimuli through repeated exposure. For instance, if a patient receives a real pain-relieving drug several times and later receives a placebo, the body may continue to respond as if the real drug is still being administered. An example of this was demonstrated by asthmatic patients who were conditioned to experience bronchodilation (expansion of the airways) in response to inhaling what they thought was a bronchodilator but was actually a harmless mist. After repeated associations between the mist and relief, the placebo alone began to produce a physiological response similar to the actual drug. This conditioned response is a testament to the learning capability of our biological systems and how they can be primed to anticipate and replicate health outcomes.
Suggestibility:
Some people are more susceptible to the placebo effect due to their inherent suggestibility. This trait allows individuals to be more easily influenced by external suggestions, such as a doctor's reassurance or the environment of a clinical setting. Clinical trials using "open-label" placebos, where patients know they are receiving a placebo but are also told that placebos can have powerful healing effects, have shown significant improvement in symptoms. This scenario highlights the power of suggestion, even when all parties are aware that the treatment has no active medical ingredients.
Individual Differences in Placebo Responsiveness
Not everyone responds to placebos in the same way. Research suggests that certain personality traits, emotional states, and cognitive processes can influence an individual's likelihood of experiencing the placebo effect. For instance, individuals who naturally possess a more optimistic outlook on life and their health outcomes tend to report greater benefits from placebo treatments. This is likely due to their higher expectancy levels, which directly influence the placebo effect through cognitive pathways that anticipate positive outcomes.
The emotional state of an individual can also influence placebo responses. Generally, higheranxiety levels can decrease the efficacy of placebo treatments, potentially due to a heightened state of physiological arousal that interferes with the mechanisms underlying the placebo effect. Conversely, being in a calm and positive emotional state can enhance responsiveness.
Moreover, the cultural context in which an individual is raised, and lives can significantly influence their belief systems about health and treatments, hence affecting placebo responsiveness. In cultures where there is a strong belief in the power of medical intervention, regardless of its nature, placebo responses tend to be stronger. In addition, the presence and perceived quality of social support can also impact how individuals respond to placebos. Supportive social environments can enhance the effectiveness of placebo treatments by reinforcing health expectations and reducing stress and anxiety.
Ethical Concerns
While there may be true benefits to using a placebo, there are also ethical concerns that need to be acknowledged. One of the primary ethical issues with the use of placebos is the potential deception involved in not disclosing to patients that they are receiving a placebo instead of an active treatment. This can affect the trust between patients and healthcare providers and conflict with the principle of informed consent. Informed consent requires that patients are fully aware of the nature of the treatment they are receiving, including any risks, benefits, and alternatives.
In medical research studies where some patients receive a placebo instead of real treatment, there's another concern that these patients might miss out on a treatment that could really help them. This issue is especially serious in situations where the patients have life-threatening or very serious conditions. Using a placebo instead of giving them proven treatments might cause their health to worsen.
Using placebos ethically means making sure that the potential harms and benefits are carefully weighed. The main reason for using placebos should be that they don't put patients at great risk, and any small risks should be worth it due to their benefits, like helping us learn about medical treatments or improving patient health when there are no other better options available.
Sources Used
1. Benedetti, F., Mayberg, H. S., Wager, T. D., Stohler, C. S., & Zubieta, J. K. (2005). Neurobiological mechanisms of the placebo effect. The Journal of neuroscience : the official journal of the Society for Neuroscience, 25(45), 10390–10402. https://doi.org/10.1523/JNEUROSCI.3458-05.2005
2. Geers, A. L., Kosbab, K., Helfer, S. G., Weiland, P. E., & Wellman, J. A. (2007). Further evidence for individual differences in placebo responding: an interactionist perspective. Journal of psychosomatic research, 62(5), 563–570. https://doi.org/10.1016/j.jpsychores.2006.12.005
3. Haour F. (2005). Mechanisms of the placebo effect and of conditioning. Neuroimmunomodulation, 12(4), 195–200. https://doi.org/10.1159/000085651
4. Jütte R. (2013). The early history of the placebo. Complementary therapies in medicine, 21(2), 94–97. https://doi.org/10.1016/j.ctim.2012.06.002
5. Munnangi S, Sundjaja JH, Singh K, et al. Placebo Effect. [Updated 2023 Nov 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513296/
6. Zhou, L., Wei, H., Zhang, H., Li, X., Bo, C., Wan, L., Lu, X., & Hu, L. (2019). The Influence of Expectancy Level and Personal Characteristics on Placebo Effects: Psychological Underpinnings. Frontiers in psychiatry, 10, 20. https://doi.org/10.3389/fpsyt.2019.00020


Comments